Are you struggling with insomnia, the most common sleep disorder? You’re not alone. An estimated 50 to 70 million people in the United States experience chronic sleep or wakefulness conditions, which are more common in females and older individuals. Poor sleep can impact focus, learning, memory, mood, and relationships with family and co-workers, and ongoing sleep issues can increase the risk of various health conditions and potentially dementia.
Fortunately, there are a range of new sleep medication options available to help you fall asleep, stay asleep, or both. Prescription sleep pills like doxepin (Silenor) and Ramelteon (Rozerem) can often relieve insomnia for short periods, while over-the-counter sleep remedies like melatonin supplements are also popular choices. However, it’s important to note that many of these medications carry risks of side effects, misuse, and dependency, and some may interact with other substances, including other medications, alcohol, and vitamin supplements.
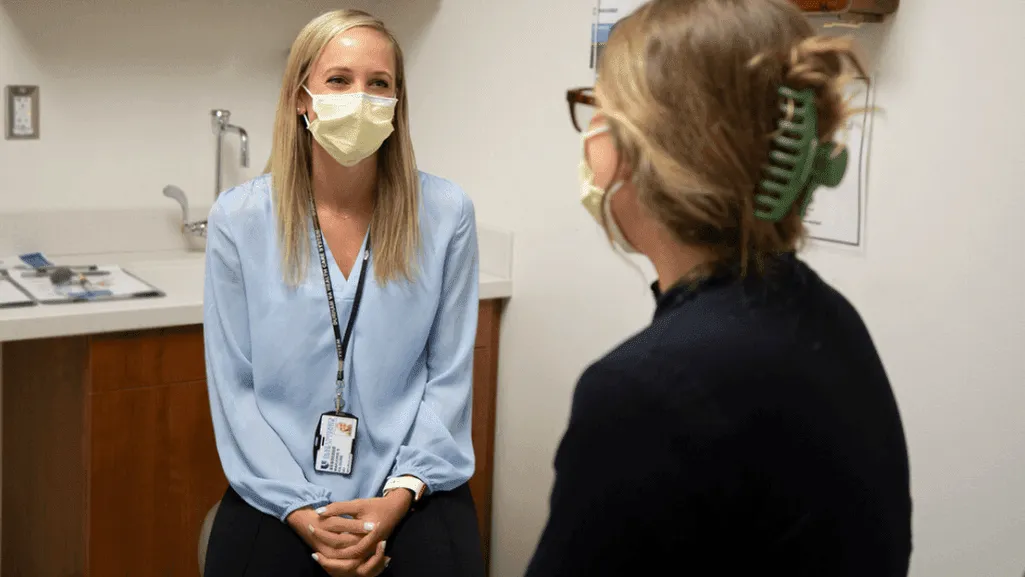
If you’re considering trying a new sleep medication, it’s crucial to consult with your doctor first to determine the best option for your specific needs and medical history. They can help you weigh the potential benefits and risks, and develop a personalized treatment plan that may include a combination of medication, cognitive behavioral therapy for insomnia (CBT-I), lifestyle changes, and sleep hygiene practices.
Key Takeaways
- Insomnia is the most common sleep disorder, affecting millions of Americans
- New sleep medication options include prescription sleep pills and over-the-counter remedies
- Medications can help with falling asleep, staying asleep, or both
- Risks of side effects, misuse, and dependency should be considered
- Consult with a doctor before starting any new sleep medication to determine the best option for your needs
The Importance of Quality Sleep for Overall Health
Getting enough quality sleep is crucial for maintaining optimal overall health and well-being. Sleep plays a vital role in allowing the body and mind to recharge, promoting physical health, mental clarity, and emotional balance. The National Sleep Foundation recommends that adults get between 7 to 9 hours of sleep per night, while children and teens require even more to support their growth and development.
Unfortunately, many individuals struggle to get the recommended amount of sleep, with 60 percent of middle schoolers and 70 percent of high schoolers not getting adequate sleep on school nights. This sleep deprivation can have serious consequences, including increased risk of motor vehicle accidents, lower grades, and poor mental health.
Physical Health Benefits of Adequate Sleep
Getting enough quality sleep is essential for maintaining physical health. During sleep, the body works to repair and regenerate tissues, build muscle, and synthesize hormones. Some of the key physical health benefits of adequate sleep include:
- Improved immune function
- Better cardiovascular health
- Enhanced muscle recovery and growth
- Increased energy levels and physical performance
- Reduced risk of obesity and diabetes
Studies have shown that individuals who consistently lack enough sleep are at higher risk for developing chronic health conditions such as heart disease, diabetes, and obesity. Even catching up on sleep during weekends may not be sufficient to reverse the negative effects of sleep deprivation on weight gain and blood sugar control.
Mental Health and Cognitive Function Improvements with Proper Sleep
In addition to the physical health benefits, getting enough quality sleep is crucial for maintaining mental health and cognitive function. During sleep, the brain processes and consolidates information, forms new neural connections, and clears out toxins. Some of the key mental health and cognitive benefits of proper sleep include:
- Improved mood and emotional regulation
- Better memory retention and recall
- Enhanced problem-solving skills and creativity
- Increased focus and productivity
- Reduced risk of depression and anxiety
Research has shown that chronic exposure to poor sleep quality is associated with an increased risk of developing mental health conditions such as depression and anxiety. Moreover, even short-term sleep deprivation can lead to irritability, mood swings, and impaired judgment and decision-making.
| Age Group | Recommended Sleep Duration |
|---|---|
| School-age children | At least 9 hours per night |
| Teens | 8-10 hours per night |
| Adults | 7 or more hours per night |
| Older adults | 7-8 hours per night |
The best bridge between despair and hope is a good night’s sleep. – E. Joseph Cossman
Prioritizing quality sleep is one of the most effective ways to improve overall health and well-being. By making sleep a top priority and implementing healthy sleep habits, individuals can unlock the numerous physical, mental, and cognitive benefits that come with a good night’s rest.
Common Sleep Disorders and Their Impact on Daily Life
Sleep disorders are a widespread issue affecting millions of people worldwide, with over 80 different types identified. Some of the most common sleep disorders include insomnia, sleep apnea, restless leg syndrome, hypersomnia, circadian rhythm disorders, and parasomnia. These disorders can significantly impact an individual’s daily life, leading to daytime fatigue, reduced cognitive function, and overall decreased quality of life.
Insomnia, characterized by difficulty falling asleep or staying asleep, affects nearly a third of the adult population, with approximately 10% experiencing severe symptoms that have daytime consequences. Women are more affected by insomnia than men, with a prevalence of 17.6% in women and 10.1% in men. Chronic insomnia can lead to mood disturbances, impaired work performance, and an increased risk of accidents.
Sleep apnea, a disorder in which breathing repeatedly stops and starts during sleep, affects millions of Americans. It can cause loud snoring, daytime sleepiness, and an increased risk of high blood pressure, heart disease, and stroke. Treatment often involves lifestyle changes, such as losing weight, and the use of continuous positive airway pressure (CPAP) therapy.
Restless leg syndrome (RLS) and periodic limb movement disorder (PLMD) are more prevalent in the elderly population. RLS causes an uncomfortable sensation in the legs and an irresistible urge to move them, which can disrupt sleep. PLMD involves repetitive leg movements during sleep, leading to fragmented sleep and daytime sleepiness.
| Sleep Disorder | Prevalence | Key Symptoms |
|---|---|---|
| Insomnia | 30% of adults; 10% severe | Difficulty falling or staying asleep |
| Sleep Apnea | 26 million Americans | Loud snoring, daytime sleepiness |
| Restless Leg Syndrome | 9% women; 5.4% men | Uncomfortable leg sensations, urge to move |
| Periodic Limb Movement Disorder | 40 per 100,000 persons | Repetitive leg movements during sleep |
Other sleep disorders, such as narcolepsy, idiopathic hypersomnia, and circadian rhythm disorders, can also significantly impact daily functioning. Narcolepsy, characterized by excessive daytime sleepiness and sudden sleep attacks, affects approximately 44.3 per 100,000 persons. Idiopathic hypersomnia, a condition causing excessive sleepiness without a known cause, has a prevalence of 10.3 per 100,000 persons.
Sleep is essential for our physical, mental, and emotional well-being. Recognizing the signs and symptoms of common sleep disorders is crucial for seeking appropriate treatment and improving overall quality of life.
If you suspect that you or a loved one may be experiencing a sleep disorder, it is essential to consult with a healthcare provider. They can help diagnose the specific disorder and recommend appropriate treatment options, such as lifestyle changes, cognitive behavioral therapy, or medication, to help improve sleep quality and daytime functioning.
Prescription Sleep Aids: How They Work and Potential Side Effects
When struggling with chronic insomnia, many individuals turn to prescription sleep aids for relief. These medications can help you fall asleep more quickly, stay asleep longer, or both. However, it’s essential to understand how these drugs work and their potential side effects before starting treatment.
Benzodiazepines for Short-Term Insomnia Treatment
Benzodiazepines, such as temazepam (Restoril), triazolam (Halcion), Ativan, Librium, Valium, and Xanax, are commonly prescribed for short-term insomnia treatment. These medications work by enhancing the effects of GABA, a neurotransmitter that promotes relaxation and sleepiness. However, benzodiazepines can be addictive and lead to substance use disorder, which is why healthcare providers usually prescribe them for short-term use only.
Benzodiazepines, such as Ativan, Librium, Valium, and Xanax, are anti-anxiety medications and can cause problems with memory and attention.
Non-Benzodiazepine Sleep Medications and Their Mechanisms of Action
Non-benzodiazepine sleep medications, also known as “Z-drugs,” include eszopiclone (Lunesta), zaleplon (Sonata), zolpidem (Ambien), and zolpidem extended-release (Ambien CR). These medications work similarly to benzodiazepines by targeting GABA receptors, but they have a different chemical structure and are less likely to cause addiction or dependence. Newer sleep-inducing medications like Ambien, Lunesta, and Sonata are less likely to be habit-forming compared to benzodiazepines.
Other prescription sleep aids include melatonin receptor agonists like ramelteon (Rozerem) and tasimelteon (Hetlioz), which work by mimicking the effects of the sleep hormone melatonin. Orexin receptor antagonists such as suvorexant (Belsomra), lemborexant (Dayvigo), and daridorexant (Quviviq) promote sleep by blocking the effects of orexin, a neurotransmitter that promotes wakefulness.
| Prescription Sleep Aid | Mechanism of Action |
|---|---|
| Benzodiazepines (e.g., Restoril, Halcion) | Enhance the effects of GABA |
| Non-Benzodiazepines (e.g., Lunesta, Sonata, Ambien) | Target GABA receptors |
| Melatonin Receptor Agonists (e.g., Rozerem, Hetlioz) | Mimic the effects of melatonin |
| Orexin Receptor Antagonists (e.g., Belsomra, Dayvigo, Quviviq) | Block the effects of orexin |
Potential Side Effects and Precautions with Prescription Sleep Aids
While prescription sleep aids can be effective in treating insomnia, they also come with potential side effects and precautions. Some common side effects include:
- Dizziness
- Headache
- Prolonged drowsiness
- Gastrointestinal problems
- Allergic reactions
- Sleep-related behaviors (e.g., sleepwalking, sleep eating)
Approximately 8 out of 10 people experience a hangover effect the day after taking sleep medicine, impacting their daily activities like driving, work, and school. Long-term use of sleeping pills can lead to dependency, rebound insomnia upon discontinuation, and potential overdosing when mixed with other sedatives or alcohol. It’s crucial to avoid mixing prescription sleeping pills with alcohol and opioids due to amplified sedative effects and potential dangers.
Certain populations should exercise caution when using prescription sleep aids:
- Pregnant or breastfeeding individuals: Sleep aids should be avoided due to the risk of passing on medication to the fetus or infant.
- Older adults: At age 65 and older, nondrug treatments are recommended as sleeping pills can increase the risk of falls and hip fractures due to side effects like confusion and memory issues.
- Individuals with chronic health conditions: Heart patients, cancer patients, and those with kidney disease or low blood pressure should consult a doctor before using sleeping pills due to potential long-term risks that may outweigh the benefits.
When considering prescription sleep aids, it’s essential to work closely with a healthcare provider to determine the most appropriate medication and dosage based on your individual needs and medical history. By understanding the potential benefits and risks associated with these medications, you can make an informed decision about your insomnia treatment plan.
New Sleep Medication: Innovative Approaches to Improving Rest
In the quest for a better night’s sleep, researchers and pharmaceutical companies have been working tirelessly to develop innovative sleep medications that target specific receptors in the brain. These groundbreaking treatments offer hope to millions of individuals struggling with insomnia and other sleep disorders, providing them with the opportunity to experience the restorative power of a good night’s rest.
Recent advancements in sleep medicine have led to the development of melatonin receptor agonists, orexin receptor antagonists, and dual orexin receptor antagonists (DORAs). These targeted therapies work by either promoting the natural sleep-wake cycle or inhibiting the activity of specific neurotransmitters that regulate wakefulness, allowing for a more balanced and restful sleep experience.
Melatonin Receptor Agonists: Ramelteon (Rozerem) and Tasimelteon (Hetlioz)
Melatonin, a hormone naturally produced by the pineal gland, plays a crucial role in regulating the body’s sleep-wake cycle. Melatonin receptor agonists, such as Ramelteon (Rozerem) and Tasimelteon (Hetlioz), work by mimicking the effects of melatonin on the brain, promoting sleep onset and maintaining a healthy circadian rhythm. These medications have shown promising results in clinical trials, with fewer side effects compared to traditional sleep aids.
Orexin Receptor Antagonists: Suvorexant (Belsomra) and Lemborexant (Dayvigo)
Orexins are neurotransmitters that promote wakefulness and regulate the sleep-wake cycle. Orexin receptor antagonists, including Suvorexant (Belsomra) and Lemborexant (Dayvigo), work by blocking the activity of orexins, thereby reducing wakefulness and allowing for a more restful sleep. These medications have demonstrated efficacy in improving both sleep onset and maintenance, making them valuable options for individuals with insomnia.
Dual Orexin Receptor Antagonists (DORAs): Daridorexant (Quviviq)
Dual orexin receptor antagonists (DORAs) represent a novel class of sleep medications that target both orexin receptors simultaneously. Daridorexant (Quviviq), a recently approved DORA, has shown remarkable effectiveness in promoting sleep onset and maintenance while minimizing the risk of side effects and dependency associated with traditional sleep aids. This innovative approach to treating insomnia offers a promising alternative for those seeking a more balanced and restorative sleep experience.
| FDA Approved Sleep Medication | Mechanism of Action | Key Benefits |
|---|---|---|
| Ramelteon (Rozerem) | Melatonin receptor agonist | Promotes sleep onset and maintains healthy circadian rhythm |
| Suvorexant (Belsomra) | Orexin receptor antagonist | Improves sleep onset and maintenance |
| Daridorexant (Quviviq) | Dual orexin receptor antagonist (DORA) | Promotes sleep onset and maintenance with reduced side effects and dependency risk |
As the landscape of sleep medicine continues to evolve, these innovative medications offer hope and relief to the millions of individuals struggling with insomnia and other sleep disorders. By targeting specific receptors and neurotransmitters involved in the sleep-wake cycle, these new treatments provide a more personalized and effective approach to improving rest and overall well-being.
Comparing the Effectiveness of New Sleep Medications to Traditional Treatments
When it comes to treating insomnia and improving sleep quality, both new sleep medications and traditional treatments offer potential benefits. However, it is crucial to understand the effectiveness and risks associated with each approach to make informed decisions about your sleep health.
According to recent studies, an estimated 35% of adults in America fail to get the recommended amount of sleep per night, with more than 8% reporting the use of a sleep aid multiple times in the previous week. While traditional treatments such as benzodiazepines and non-benzodiazepine hypnotics have been widely used, newer medications like orexin receptor antagonists and melatonin receptor agonists are gaining popularity for their targeted approach to treating insomnia.
Z drugs, a class of non-benzodiazepine hypnotics, are approved by the FDA for short-term therapy for insomnia. These medications can help with both falling asleep and staying asleep throughout the night. However, studies show that women are frequently more affected than men by Z drugs, increasing the risks of impairment the next day. In contrast, orexin receptor antagonists are approved for the treatment of insomnia related to both sleep onset and sleep maintenance, offering a more comprehensive approach to managing sleep disorders.
Ramelteon, a melatonin receptor agonist, is another new sleep medication approved by the FDA to treat insomnia related to initially falling asleep. While most people can use ramelteon safely, it should not be used by individuals with sleep maintenance insomnia and should be cautiously used by those with other health conditions that could be influenced by the drug.
When comparing the effectiveness of new sleep medications to traditional treatments, it is essential to consider the unique needs of each individual. The following table highlights some key differences between these two approaches:
| Traditional Treatments | New Sleep Medications |
|---|---|
| Benzodiazepines and non-benzodiazepine hypnotics | Orexin receptor antagonists and melatonin receptor agonists |
| Short-term relief from insomnia | Targeted approach to treating specific aspects of insomnia |
| Potential for side effects, dependency, and rebound insomnia | Generally well-tolerated with fewer side effects |
| May cause impairment in cognitive function and motor skills | Minimal impact on cognitive function and motor skills |
While new sleep medications offer promising results in terms of effectiveness and safety, it is crucial to discuss the options with a healthcare provider before starting any treatment. By considering factors such as sleep patterns, overall health, and potential side effects, individuals can work with their doctor to develop a personalized approach to improving sleep quality and enhancing overall well-being. Non-pharmacological approaches, such as cognitive-behavioral therapy for insomnia (CBT-I) and lifestyle changes, can also play a significant role in promoting healthy sleep habits and reducing the need for long-term medication use.
“The effectiveness of new sleep medications compared to traditional treatments varies depending on the individual’s specific needs and health condition. It is essential to work closely with a healthcare provider to determine the most appropriate course of action for improving sleep quality and overall well-being.” – Dr. Sarah Thompson, Sleep Medicine Specialist
As research continues to advance our understanding of sleep disorders and their underlying mechanisms, the future of sleep medicine holds promise for the development of even more targeted and effective treatments. By staying informed about the latest advancements in sleep medication and working closely with healthcare professionals, individuals can take proactive steps towards achieving the restful, restorative sleep they need to thrive.
Non-Pharmacological Approaches to Enhancing Sleep Quality
While prescription sleep aids can provide relief for those struggling with chronic insomnia, non-pharmacological approaches offer a safe and effective alternative for improving sleep quality. These methods focus on addressing the underlying causes of sleep disturbances and promoting healthy sleep habits without relying on medication.
According to a study by Aparício et al. (2020), non-pharmacological interventions were found to improve inpatients’ sleep quality in intensive care units and acute wards. These interventions encompass a range of techniques, including cognitive behavioral therapy, lifestyle modifications, and complementary and alternative medicine.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
Cognitive behavioral therapy for insomnia (CBT-I) is a structured program that helps individuals identify and change thoughts and behaviors that interfere with sleep. This therapy focuses on educating patients about sleep, establishing a consistent sleep schedule, and developing relaxation techniques to reduce anxiety and promote restful sleep.
“CBT-I is a safe and effective treatment for chronic insomnia, with long-lasting results. It should be the first-line treatment for adults with chronic insomnia.” – American Academy of Sleep Medicine
Lifestyle Changes and Sleep Hygiene Practices
Adopting healthy lifestyle habits and practicing good sleep hygiene can significantly improve sleep quality. Some essential sleep hygiene practices include:
- Maintaining a consistent sleep schedule
- Creating a comfortable sleep environment
- Avoiding caffeine, alcohol, and heavy meals before bedtime
- Engaging in regular exercise
- Managing stress through relaxation techniques
A study by Faraklas et al. (2013) observed a positive impact of a nursing-driven sleep hygiene protocol on sleep quality in burn care patients, highlighting the importance of these practices in promoting restful sleep.
Complementary and Alternative Medicine (CAM) for Sleep Improvement
Complementary and alternative medicine (CAM) offers various non-pharmacological approaches to enhancing sleep quality, such as:
- Acupuncture
- Massage therapy
- Meditation and mindfulness practices
- Herbal remedies (e.g., valerian root, chamomile)
- Aromatherapy
Garcia et al. (2018) reported on the benefits of inpatient acupuncture at a major cancer center for sleep enhancement, while Hajibagheri et al. (2014) found that Rosa damascene aromatherapy significantly improved sleep quality in cardiac patients in a randomized controlled trial.
| Non-Pharmacological Approach | Key Benefits |
|---|---|
| Cognitive Behavioral Therapy for Insomnia (CBT-I) | Identifies and changes thoughts and behaviors that interfere with sleep |
| Lifestyle Changes and Sleep Hygiene Practices | Promotes healthy habits and creates a conducive sleep environment |
| Complementary and Alternative Medicine (CAM) | Offers various techniques to enhance relaxation and improve sleep quality |
By incorporating these non-pharmacological approaches into a comprehensive sleep management plan, individuals can effectively improve their sleep quality and overall well-being without relying solely on medication.
Discussing New Sleep Medication Options with Your Healthcare Provider
When struggling with persistent sleep issues, it’s essential to discuss your concerns with a healthcare provider. They can help identify the underlying causes of your insomnia and recommend the most appropriate treatment options, including new sleep medications. By working closely with your doctor, you can find the best solution to improve your sleep quality and overall well-being.
When to Seek Professional Help for Sleep Issues
If you’ve been experiencing sleep problems for more than a few weeks, it’s time to consult your healthcare provider. Chronic insomnia affects 10% of the adult population, and seeking professional help is crucial for proper management. Your doctor can assess your sleep patterns, medical history, and any underlying conditions that may be contributing to your insomnia. They can then recommend the most suitable treatment plan, which may include new sleep medications, cognitive behavioral therapy, or lifestyle changes.
Providing a Comprehensive Medical History and Sleep Diary
To help your healthcare provider make an accurate diagnosis and develop an effective treatment plan, it’s important to provide them with a comprehensive medical history and sleep diary. This information can help identify any underlying medical conditions, such as kidney disease, liver problems, or low blood pressure, which may impact the safety and effectiveness of certain sleep medications. Your sleep diary should include details about your sleep patterns, duration, and any factors that may be disrupting your rest.
| Key Information to Share with Your Healthcare Provider | Importance |
|---|---|
| Medical history | Helps identify underlying conditions that may affect sleep medication safety and effectiveness |
| Current medications | Allows your doctor to assess potential drug interactions and side effects |
| Sleep diary | Provides valuable insights into your sleep patterns, duration, and disruptive factors |
| Lifestyle factors | Helps your doctor identify areas for improvement, such as sleep hygiene and stress management |
When discussing sleep medication options with your healthcare provider, it’s essential to ask questions and express any concerns you may have. Your doctor can provide guidance on the potential benefits and risks of each treatment, as well as the appropriate dosage and duration of use. By working together, you can develop a personalized plan to improve your sleep quality and enhance your overall health and well-being.
The Future of Sleep Medicine: Emerging Therapies and Research
As we look towards the future of sleep medicine, a myriad of exciting developments and emerging therapies are on the horizon. Sleep researchers and clinicians are tirelessly working to uncover novel drug targets, explore innovative treatment approaches, and harness the power of personalized medicine to revolutionize the way we diagnose and manage sleep disorders.
One promising avenue in the future of sleep medicine is the identification of novel drug targets and mechanisms of action. By delving into the complex neurobiological pathways that regulate sleep and wakefulness, scientists are uncovering potential targets for new medications. For instance, recent research has shed light on the role of orexin receptors in modulating sleep-wake cycles, leading to the development of dual orexin receptor antagonists (DORAs) like daridorexant (Quviviq) for the treatment of insomnia.
Novel Drug Targets and Mechanisms of Action
In addition to orexin receptors, researchers are exploring other novel drug targets, such as melatonin receptors, GABA receptors, and histamine receptors. By targeting these specific receptors, scientists aim to develop more targeted and effective sleep medications with fewer side effects compared to traditional treatments. Moreover, emerging therapies are focusing on non-pharmacological approaches, such as neurostimulation techniques and phototherapy, which hold promise for improving sleep quality without relying on medication.
Personalized Medicine Approaches to Sleep Disorder Treatment
Another exciting frontier in the future of sleep medicine is the rise of personalized medicine approaches. With advancements in genomics, wearable technology, and data analytics, clinicians are increasingly able to tailor sleep disorder treatments to individual patients based on their unique genetic makeup, lifestyle factors, and sleep patterns. Genomic studies, such as those conducted in the UK Biobank, have identified genes like PAX8 that influence sleep duration, showcasing the genetic factors affecting sleep health.
The use of wearable devices, mobile health applications, and advanced diagnostic tools in personalized sleep medicine is rapidly increasing. These technologies enable clinicians to gather real-time data on patients’ sleep patterns, monitor treatment progress, and make data-driven decisions to optimize care. Telemedicine has also emerged as a valuable tool in sleep medicine, with studies showing increased adherence to continuous positive airway pressure (CPAP) therapy and improved patient outcomes.
| Telemedicine Intervention | Effect |
|---|---|
| Average daily CPAP usage | Increased by 36 minutes (weighted mean difference: 0.61, 95% CI: 0.39 to 0.83) |
| Percentage of days with CPAP usage >4 hours | Increased by 10.67% |
| Daytime sleepiness | Decreased (weighted mean difference: -0.26, 95% CI: -0.79 to 0.28) |
| Apnea-hypopnea index (AHI) reduction | -0.53 (95% CI: -3.58 to 2.51) |
| Overall quality of life (standardized mean difference) | -0.25 (95% CI: -0.25 to 0.76) |
As we embrace the future of sleep medicine, it is crucial for healthcare providers to stay informed about emerging therapies and research developments. By incorporating novel drug targets, personalized medicine approaches, and innovative technologies into clinical practice, we can enhance the diagnosis, treatment, and management of sleep disorders, ultimately improving the lives of countless individuals suffering from sleep-related issues.
Conclusion
In today’s fast-paced world, improving sleep quality has become a top priority for many individuals. With up to 80% of the population experiencing transient insomnia and 15% dealing with chronic insomnia, it’s clear that sleep disorders are a widespread issue. Fortunately, recent advancements in sleep medicine have provided us with a range of prescription medications, such as doxepin, ramelteon, suvorexant, and daridorexant, which can help alleviate these problems and promote more restful sleep.
However, it’s crucial to remember that these medications may come with potential side effects and risks. For example, suvorexant has been shown to cause dose-dependent somnolence in trials, with a reported 7% incidence rate compared to 3% placebo. Additionally, it may lead to next-day impairment, cognitive and behavioral changes, and even a dose-dependent increase in suicidal ideation. Therefore, before starting any new sleep aid, it is essential to consult a healthcare provider who can assess your individual needs and recommend the most suitable treatment plan.
In addition to pharmacological interventions, non-pharmacological approaches such as cognitive behavioral therapy, lifestyle changes, and complementary and alternative medicine can also be highly effective in enhancing sleep quality. By combining treatments tailored to your specific needs and circumstances, you can work towards achieving the restful, restorative sleep your body and mind crave. As research continues to uncover novel drug targets and personalized treatment approaches, the future of sleep medicine looks brighter than ever. So, if you’re struggling with sleep issues, don’t hesitate to reach out for help – a better night’s sleep may be just around the corner.